Medical Review By: Rachelle Lacey, MD
White spots on the skin are usually a cosmetic problem. They can be just as noticeable and bothersome as dark spots, and they may itch, but in most cases they are harmless. That said, whenever you notice a change in your skin, it’s always smart to see a dermatologist.
Here are a few of the skin conditions that can cause white spots on the skin.
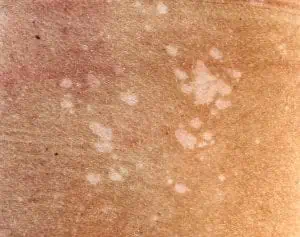
(pictured to the right: Arm with idiopathic guttate hypomelanosis)
Idiopathic guttate hypomelanosis
Sometimes referred to as “reverse freckles,” idiopathic guttate hypomelanosis (IGH) is a condition in which small (1 to 5 millimeter) flat spots of white skin called hypopigmented
macules develop. They commonly appear on sun-exposed areas, such as the legs and forearms. The risk of developing IGH increases with age; most people who have it are over 40.
The cause of IGH is unknown, though factors such as chronic sun exposure and genetics may play a role. People with fair skin are more prone to IGH, but the patches are more noticeable on dark skin.
How it’s treated: The macules are benign and don’t have to be removed. A consistently effective treatment has yet to be discovered. Cryotherapy is sometimes used, with mixed results. In some cases, the cryotherapy itself can cause light or dark spots. Practicing sun protection, including using a broad-spectrum sunscreen with SPF 30 or more and wearing protective clothing, can help prevent the spots from becoming more noticeable and also help prevent new spots from forming.
Milia

The bumps, which can also be yellowish, usually form when dead skin cells build up under the top layer of the skin. They are more common in people who have acne and blackheads. Other causes include an injury to the skin, such as a burn, sunburn or blistering rash, and using topical corticosteroids for a long period.
How it’s treated: Milia are harmless and don’t need treatment. They may go away on their own, but if they don’t, your skin care provider can remove them. (You can’t “pop” them like a pimple.) Treatment options include chemical peels, dermabrasion, laser ablation, deroofing (removing the top of the cyst with a needle or small scalpel and extracting the contents) and cryotherapy (freezing).
Tinea versicolor
The condition is more common in teenagers and young adults and typically affects the torso and shoulders. Triggers include hot and humid weather, oily skin, hormone changes and a weak immune system.
How it’s treated: Cleansing the affected areas with dandruff shampoo and using an anti-fungal cream or taking anti-fungal medication can help restore your normal pigmentation, though it can take several months after beginning treatment for the normal skin color to return. Tinea versicolor often recurs, so your doctor may recommend maintenance treatments to prevent it from coming back.
Pityriasis alba

How it’s treated: Pityriasis alba may go away on its own, though it can take several years to do so. Petroleum jelly or a moisturizer with emollients can lessen any scaling. If the skin is also inflamed, red and itchy, see your dermatologist. The doctor may recommend using a corticosteroid cream or a non-steroidal cream.
Vitiligo

The loss of color occurs when cells that produce melanin, skin’s natural pigment, die or stop working. It’s not clear what triggers vitiligo, but it may be an autoimmune disease in which the body attacks its own pigment-making cells. Genetics may play a role. There is also an association between thyroid disease, diabetes and vitiligo. Sometimes, a severe sunburn, skin trauma or a period of severe emotional stress can trigger vitiligo or make it worse.
How it’s treated: Vitiligo doesn’t threaten a person’s physical health but it can cause emotional distress. There is no cure, but some treatments aim to restore normal skin color. These include anti-inflammatory creams, oral corticosteroids and forms of light therapy called psoralen plus ultraviolet-A (PUVA) and narrow band UV-B (NB-UVB). If other treatments don’t work, surgery in the form of skin grafting or pigment cell grafting may be a course of last resort. An experimental treatment in the form of an oral medication known as a JAK inhibitor is currently in the works. The medication could improve vitiligo by tamping down the immune system.
Lichen sclerosus

The causes of lichen sclerosus aren’t well understood, but it may be the result of genetics, an overactive autoimmune system, hormone imbalances or an injury that damages or scars the skin.
How it’s treated: If you suspect you have lichen sclerosus, see your doctor. Lichen sclerosus needs to be treated because the patches can scar and interfere with urination and sex. There’s also a very small chance that the patches could become cancerous. Corticosteroid creams and ointments are the most common form of treatment. Children who develop lichen sclerosus are often fortunate enough to outgrow the condition.
No matter the cause of your white spots, if they appear in areas that see the sun, reducing sun exposure and wearing sunscreen is critically important.
Article Written By: Jessica Brown is a health and science writer/editor based in Brooklyn, New York. Her work has appeared in Prevention, Johnson & Johnson, the Breast Cancer Research Foundation and many more